Mast Cell Activation Syndrome: How To Calm A Hyperactive Immune System
Life’s challenging enough when you have one or two food allergies and maybe an environmental allergy. No bread because of gluten, no regular pizza because of dairy, and come springtime when the flowers are blooming you stay inside because pollen triggers miserable sneezing attacks.
But if you have Mast Cell Activation Syndrome (MCAS), it makes it seem like being sensitive to just a few things is a walk in the park. MCAS is an extreme overreaction of the immune system and the disorder just might be more common than many health professionals realize.
If you have multiple undiagnosed, unexplainable allergic symptoms, you may have MCAS.
This article will cover:
- What is Mast Cell Activation Syndrome?
- What causes MCAS?
- Symptoms of MCAS
- The connection between Lyme disease and MCAS
- Who is at risk for MCAS?
- How to reduce MCAS symptoms
- Foods to avoid
- Coping mechanisms
What is Mast Cell Activation Syndrome?
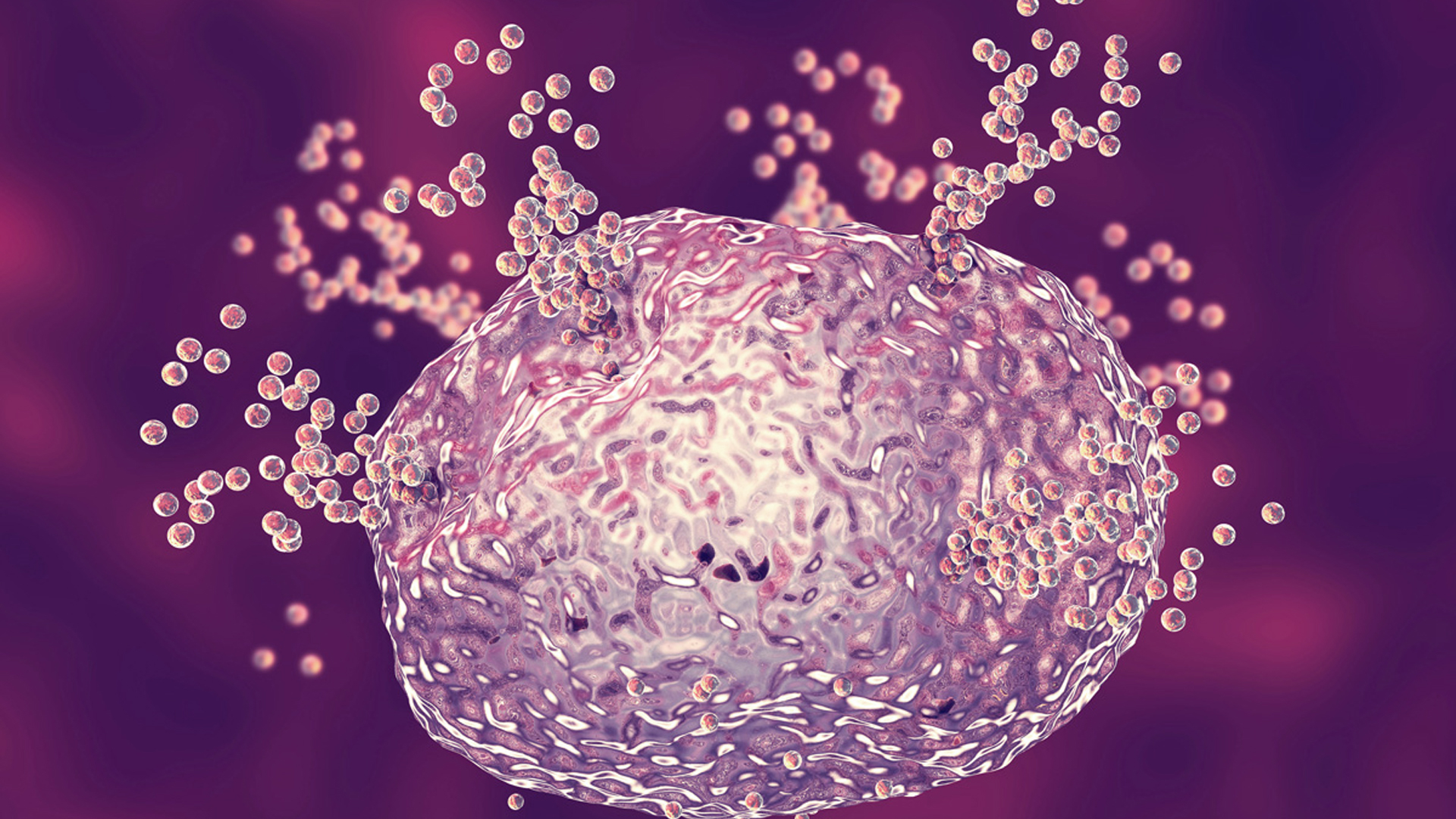
T.C. Theoharides Ph.D., M.D, is a leading authority on MCAS (his website: MastCellMaster.com). Dr. Theoharides explains that mast cells are the “universal alarm cells” that kickstart a cascade of inflammatory responses.
So far, so good, because mast cells, which are white blood cells, are a normal part of the immune system. Imagine a house with thousands of alarm sensors in every nook and cranny of the home. That’s essentially what mast cells are in the body. Each organ and every sinew and connective tissue in the body contains mast cells.
The job of mast cells is to sound the alarm when stress is detected, be it in the form of an infection, an environmental trigger, toxins, or an injury. When these stressors are detected, mast cells release chemicals such as histamine which trigger an immune response.
Again, all good because properly-functioning mast cells help us physically deal with stress. But—and for people with MCAS, it’s a huge but—some people have overactive mast cells. This hypersensitivity can lead to autoimmune responses; the body starts attacking itself.
Although mast cells are located throughout the body, they are most prevalent in organs that have a direct line to the outside world. Think nasal passages, the lungs, skin, and the GI tract, which is home to up to 80% of immune cells.
Is MCAS Common?
According to Dr. Todd Maderis, many people (including physicians) mistakenly refer to the symptoms caused by MCAS as histamine intolerance. Although histamine is the most common mast-cell mediator, it’s not the only one. (If you’re keeping score at home, other mediators include: neutral proteases, proteoglycans, and cytokines such as tumor necrosis factor-alpha).
So if unexplainable symptoms are not caused by an intolerance to histamine, then what’s the explanation? Dr. Maderis suggests that MCAS is the cause. Although the disease is thought to be rare, a research study in the Journal of Hematology & Oncology says, “Recent findings suggest MCAS is a fairly common disorder.”
The good news is that having MCAS isn’t a life sentence. By being vigilant about eliminating potential inflammatory triggers, people with MCAS can live a mostly symptom-free life. The path isn’t easy but it’s doable. (See below.)
Symptoms of MCAS
It would be easier to include a list of symptoms not related to MCAS. Virtually every system of the body can be affected by the overactive immune response, including:
- Digestive: Pretty much any symptom associated with leaky gut (which may be a trigger of MCAS, or vice versa) – abdominal cramps, indigestion, diarrhea, acid reflux, as well as nausea and vomiting.
- Cognitive: Brain fog, difficulty concentrating, and diminished memory.
- Mood: Anxiety and depression, mood swings
- Skin: Rashes, itching, dryness, hives, redness
- Respiratory: Wheezing, congestion, difficulty breathing, difficulty swallowing
- Musculoskeletal: Joint pain, reduced bone density, muscle aches
- Cardiovascular: Hypertension, fainting, arrhythmia
- Miscellaneous: Headaches, chronic fatigue, urinary tract infections
People living with certain chronic diseases may also have MCAS. Or, it’s possible that having MCAS triggers a certain chronic disease. Researchers have yet to solve this chicken-or-egg scenario.
The Connection Between MCAS and Lyme Disease
One of the best examples of this chicken vs egg scenario is Lyme Disease, the tick-borne illness caused by Borrelia burgdorferi, a bacteria carried by deer ticks that when transmitted to humans can cause joint pain, fatigue, and flu-like symptoms.
The overreaction of mast cells can trigger and exaggerate Lyme Disease symptoms; symptoms of MCAS overlap with Lyme Disease. At least one research study confirms that Borrelia burgdorferi triggers mast cell hyperactivity.
The aforementioned Dr. Maderis, a renowned Lyme Disease expert, says “It is important to test for Lyme disease and associated infections to determine if the infections are driving the mast cell mediator release.”
Dr. Marty Ross, M.D., who operates TreatLyme.net, explains that Lyme Disease causes mast cells to release histamine more easily. The pernicious thing about Lyme Disease is that mast cells can become activated even absent the presence of an allergic trigger.
Who is at Risk of Developing MCAS?
A study in the American Journal of the Medical Sciences examined 400 patients with MCAS and identified the prevalence of specific characteristics. Women made up 69% of patients with mast cell activation syndrome, and 75% were Caucasian. The most frequent age at onset of symptoms was nine years old, and in most patients, it took 30 years to get a diagnosis of MCAS. “This implies people with MCAS may spend a good portion of their life without a proper diagnosis,” the researchers concluded.
Testing for MCAS is available, however, a negative test may be false and should not rule out the possibility of having the disorder, says the American Academy of Allergy, Asthma & Immunology.
A review in the Journal of Hematology & Oncology recommends that MCAS should be considered as a diagnosis in patients with “chronic multisystem polymorbidity or patients in whom a definitively diagnosed major illness does not well account for the entirety of the patient’s presentation.”
How to Reduce MCAS Symptoms

In order to lessen the chances of experiencing auto-inflammatory episodes, it’s going to take a lot of work. But the first step is to confirm if you have MCAS in the first place. And the best way to do that is to get tested for genetic defects that are common in people with MCAS.
A couple of examples of genetic defects to get tested for include MTHFR (which indicates an inability to clear histamine) and KIT-D816V (having this defect suggests that there is a continuous activation of mast cells).
An obvious remedy for MCAS is antihistamines. (For best results, have a medical professional recommend one for you.)
Lonnie Marcum, a Licensed Physical Therapist and mother of a daughter who had a near-death experience with Lyme Disease but is now mostly symptom-free, runs the blog, LymeSci on LymeDisease.org. Here’s how Marcum helped her daughter:
- Treat for infections (bacteria, fungi, parasites, viruses)
- Avoid or quickly treat insect bites (spiders, ticks, fleas, mosquitos, bed bugs)
- Eliminate stress foods (dairy, fermented or aged foods, wheat, shellfish, sugar, and preservatives)
- Avoid drugs (alcohol, hormones, antibiotics, anesthetics, opioids, aspirin, NSAIDs, excipients)
- Don’t use artificial dyes (food coloring, radiographic dyes, pigments in makeup)
- Limit exposure to environmental toxins (pollen, dust, mold, animal dander, heavy metals, pesticides)
- Cover the nose or use a mask when confronted with noxious odors (perfumes, smoke, exhaust fumes, smog)
What To Eat And Avoid For MCAS
According to Marcum, her daughter’s health vastly improved by eating a “basic, clean diet,” consisting of fresh food with nothing cured, processed or fermented. The diet must be from organic food and gluten-free, dairy-free, dye-free, sugar-free, low-histamine, low-citrus, low-oxalate, and low-nightshade, says Marcum.
In addition, Dr. Marty Ross recommends two supplements that may help stabilize mast cells so they do not release their chemicals: Quercetin, at a dose of 250 mg, two or three times a day, and Luteolin at a dose of 100 mg two or three times a day.
Healing From MCAS
It’s always a good idea to maintain a spiritual practice that focuses on health-consciousness, and being an active participant in your health journey.
In addition, if you suspect you have MCAS or a test has confirmed it, you’ll want to seek a physician who is very knowledgeable about it as well as related conditions such as Lyme Disease.
Dealing with the multiple symptoms induced by MCAS is very challenging. For this reason, you may need extra support. Talk to a psychologist. Get massages or visit a chiropractor. Visit an Innovative Medicine professional.
Disclaimer: The statements made in this article have not been evaluated by the Food and Drug Administration. Any products or treatments mentioned are not intended to diagnose, treat, cure, or prevent any disease. Please consult a licensed medical practitioner for medical advice.
At Innovative Medicine, we believe in transparency. We want you to know that we may participate in affiliate advertising programs pertaining to products mentioned herein.
See how we can help you restore complete health of body, mind & spirit.
Join our mailing list and receive exclusive offers + information!





Leave a Reply
Want to join the discussion?Feel free to contribute!